Endometriosis is a chronic condition where tissue similar to the lining inside the uterus grows outside of it, causing pain and other symptoms. It can affect fertility and quality of life but is often underdiagnosed or mistaken for other issues.
Understanding endometriosis is essential because many people suffer in silence without proper diagnosis or treatment. Its symptoms vary widely, making awareness and medical guidance key to managing the condition effectively.
This article explores what endometriosis is, common symptoms, and available treatment options to inform those seeking answers or support.
Table of Contents
What Is Endometriosis?

Endometriosis is a chronic medical condition involving the growth of tissue similar to the uterine lining outside the uterus. It causes pain and may affect fertility. Understanding its nature, who it impacts, and how common it is helps clarify why timely diagnosis and treatment matter.
Definition and Overview
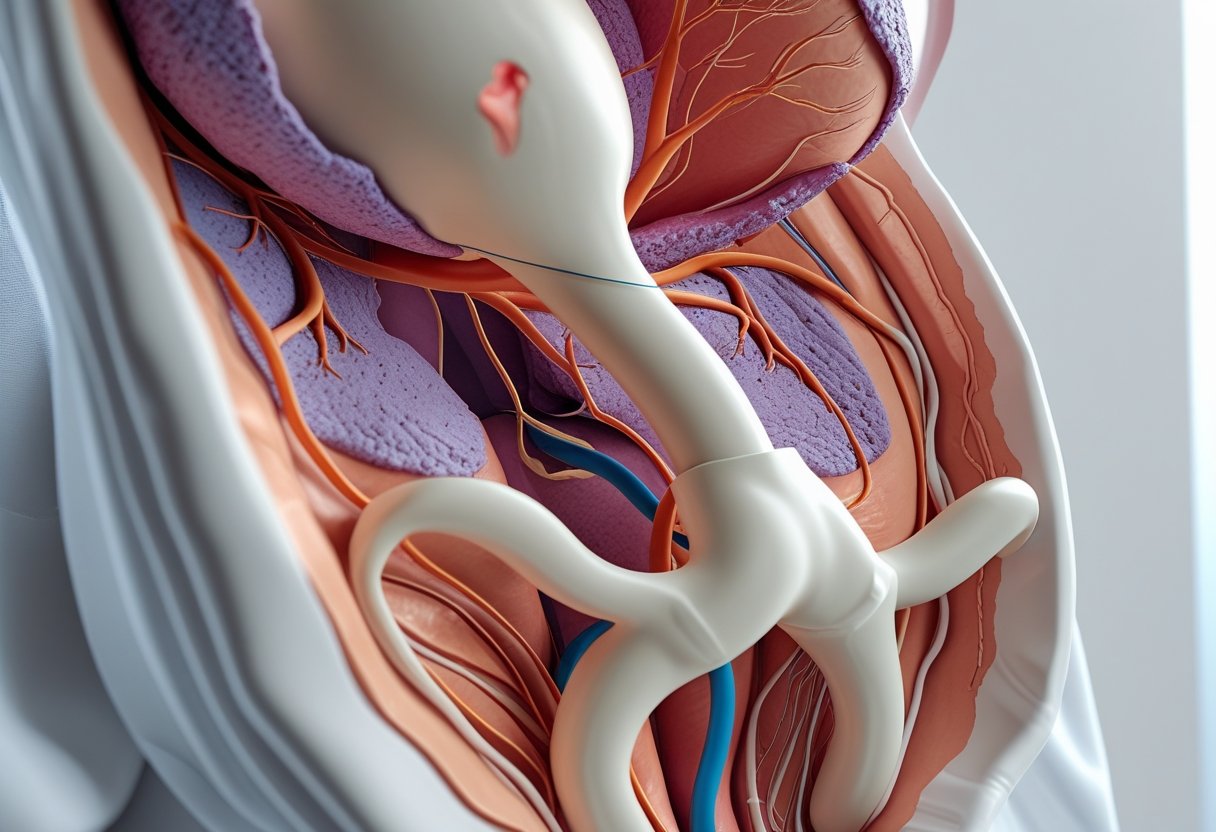
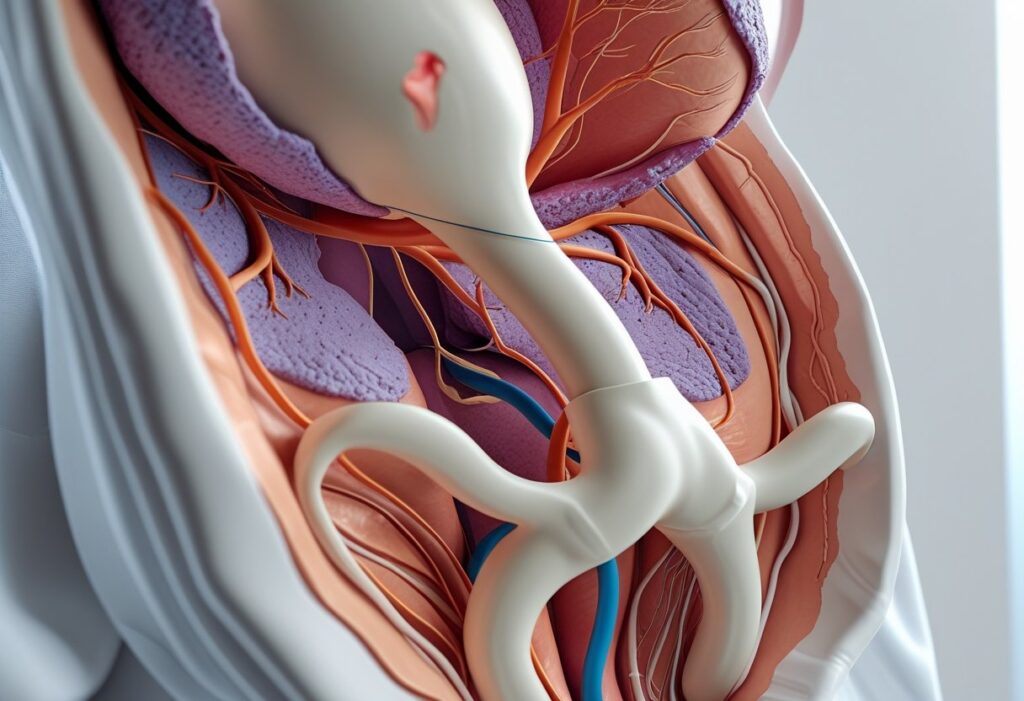
Endometriosis occurs when tissue resembling the endometrium grows outside the uterus on organs such as ovaries, fallopian tubes, and pelvic lining. This misplaced tissue thickens, breaks down, and bleeds with each menstrual cycle.
Unlike the normal uterine lining, this tissue has no way to exit the body, leading to inflammation, pain, and scar tissue formation. Symptoms vary but often include severe menstrual cramps, pelvic pain, and pain during intercourse.
Who Is Affected
Endometriosis primarily affects individuals assigned female at birth, typically during reproductive years (ages 15 to 49). It can appear soon after menstruation begins and may persist until menopause.
Though anyone with a uterus can develop it, certain factors increase risk, including family history, short menstrual cycles, and low body mass index. Symptoms can significantly impact quality of life, causing physical discomfort and emotional distress.
Prevalence and Statistics
Estimates suggest endometriosis affects about 10% of women of reproductive age globally. In the United States, roughly 6 to 10 million women experience the condition.
Diagnosis often takes 7 to 10 years from symptom onset due to symptom overlap with other disorders and reliance on surgical confirmation. It is one of the leading causes of infertility, affecting up to 30-50% of those with the condition.
Common Symptoms of Endometriosis

Endometriosis presents with several distinct symptoms impacting daily life and reproductive health. The primary complaints often involve pain, irregular menstrual cycles, and persistent tiredness, affecting physical and emotional well-being.
Pelvic Pain
Pelvic pain in endometriosis is often chronic and can vary from mild to severe. It typically occurs before and during menstruation but may also be present throughout the month.
This pain results from the growth of endometrial-like tissue outside the uterus, causing inflammation and irritation of surrounding organs. It may include sharp cramping, dull aching, or stabbing sensations, especially in the lower abdomen and lower back.
Pain can also arise during or after sexual intercourse, bowel movements, or urination. Such symptoms help differentiate endometriosis pain from other pelvic disorders.
Menstrual Irregularities
Menstrual changes are common with endometriosis and vary widely among individuals. Heavy menstrual bleeding (menorrhagia) is frequent, often accompanied by prolonged periods lasting longer than seven days.
Some women experience spotting between cycles or irregular cycles with unpredictable timing. Painful periods with intense cramping (dysmenorrhea) are another hallmark, severely impacting quality of life.
These menstrual irregularities may contribute to anemia and fatigue due to excessive blood loss. Tracking cycle patterns can aid diagnosis and management.
Fatigue
Fatigue related to endometriosis is often severe and persistent. It extends beyond feeling tired and can impair concentration, motivation, and physical endurance.
This symptom may be caused by chronic pain, inflammation, and disrupted sleep patterns due to discomfort. Additionally, fatigue is sometimes linked to anemia from heavy menstrual bleeding.
Fatigue reduces daily functioning and lowers overall energy levels, making symptom management a priority in treatment plans.
Causes and Risk Factors

Endometriosis develops from multiple factors that interact in complex ways. These include inherited traits, hormone levels, and external influences from the environment.
Genetic Predisposition
Research shows that endometriosis tends to run in families, indicating a hereditary component. Women with a first-degree relative who has the condition are three to nine times more likely to develop it themselves.
Several genes related to immune response and hormone regulation are being studied for their role. However, no single gene is responsible; rather, multiple genes seem to increase susceptibility.
Genetic predisposition alone does not cause endometriosis but raises the likelihood when combined with other factors.
Hormonal Influences
Estrogen, a key female hormone, plays a central role in endometriosis. It promotes the growth and maintenance of endometrial tissue, including the abnormal implants outside the uterus.
Women with endometriosis often show increased local production of estrogen in lesions. This hormone imbalance encourages inflammation and slows lesion regression.
Progesterone resistance is also observed, reducing the hormone’s ability to counteract estrogen’s effects. These hormonal changes contribute to persistent and painful symptoms.
Environmental Factors
Certain environmental exposures may increase the risk of endometriosis. Chemicals like dioxins and polychlorinated biphenyls (PCBs) disrupt immune and hormonal systems.
Lifestyle aspects like diet and exposure to toxins could play a role, but evidence is still limited. Smoking, alcohol use, and high caffeine intake show inconsistent links.
Early age at menstruation and short menstrual cycles increase risk due to longer estrogen exposure. Immune system dysfunction also contributes by failing to clear displaced tissue effectively.